- You are here:
- Home
- Focus Areas
Oral health was cited as the greatest unmet health need for U.S. children, disproportionately affecting the nation’s poorest children. Although preventable, dental caries (tooth decay) is among the most prevalent chronic conditions in U.S. children. Untreated caries can lead to pain, infection, problems with eating and speaking, and missed school days.
What We Do
Medicaid Population Study
State-level interventions and policies have targeted improvements in utilization of dental care services in response to the Department of Health and Human Services Oral Health Initiatives. However, such interventions and policies have not led to an increase in preventive oral healthcare utilization at the rate suggested by the Oral Health Initiative of the Centers for Medicare & Medicaid Services, which can only be achieved with targeted and local interventions.
In our research, we analyze the dental care provision for Medicaid-enrolled children derived from the Medicaid Analyic eXtract (MAX) claims data towards data-informed recommendations of local and population targeted interventions for improving the uptake of preventive dental care among these children.
Access to Preventive Dental Care for Children
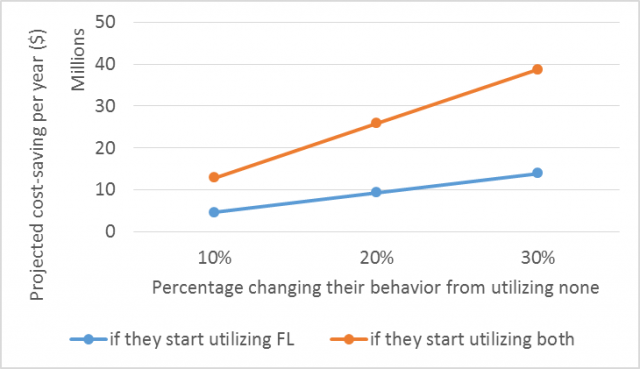
Potential Cost-savings for Texas at different penetration levels of preventive dental care for young children
Public insurance programs such as Medicaid/CHIP remove many barriers related to financial access for dental care receipt for children with public insurance; other forms of access impact the utilization of dental care services to a greater extent. Public insurance programs such as Medicaid/CHIP remove many barriers related to financial access for dental care receipt for children with public insurance; other forms of access impact the utilization of dental care services to a greater extent. The Centers for Medicare and Medicaid Services (CMS) identified several barriers to dental care, including limited availability of dental providers and low reimbursement rates. According to a 2009 survey, identifying a dentist accepting Medicaid remained the most frequently reported barrier to children seeking dental services. These barriers reflect two dimensions of access, accessibility (i.e., distance to a provider) and availability (i.e., scarcity of providers), collectively referred to as spatial access.
In our research, we develop mathematical models for estimating access to dental care accounting for provider capacity and Medicaid capacity for those provides participating in the public insurance program as well as for the need for dental care differentiated between preventive and restorative care, by age and by risk of caries. The models can be used to simulate ‘what-if-scenarios’ such as changes in policies, in the access network or other system levelers that are known to influence access.
Cost-Saving of Preventive Dental Care for Young Children
Basic pediatric dental preventive services include dental prophylaxis (teeth cleaning), topical fluoride application, and dental sealants. There is no evidence that dental prophylaxis is effective in preventing dental caries. In contrast, there is strong evidence that the application of dental sealants and topical fluoride are effective prevention services. The American Academy of Pediatric Dentistry recommends application of dental sealants and topical fluoride as part of a comprehensive prevention strategy. Further, several studies have found that fluoride varnish applied in medical settings prevents caries and is cost-effective. While there is evidence for the effectiveness of preventive dental care, there is no consensus on how those prevention services impact downstream dental care expenditures and outcomes.
In our research, we assess how topical fluoride treatments and dental sealants (either primary or permanent molars) together impacted overall downstream dental care expenditures and outcomes by using multi-year longitudinal utilization for dental care derived from patient-level claims. To estimate the impact of utilization behaviors on associated costs, we cluster patient-level data derived from the Medicaid Analytic Extract (MAX) claims files based on the utilization of topical fluoride and sealants before restorative care treatment was provided. Using patient-level detailed utilization data over multiple years, we determine the temporal relationship between preventive and restorative dental care.
Publications
Georgia Tech Contributors
Journals
Lee, I., Monahan, S., Serban, N., Griffin, P., Tomar, S. (2017) Estimating the Cost Savings of Preventive Dental Services Delivered to Medicaid-Enrolled Children in Six Southeastern States, Health Services Research, in press.
Serban, N., Tomar, S. (Accepted June 2018) ADA Health Policy Institute’s Methodology Overestimates Spatial Access to Dental Care for Publicly Insured Children, Journal of Public Health Dentistry, in press.
Johnson, B., Serban, N., Griffin, P., Tomar, S. (Submitted March 2018) Does Silver Diamine Fluoride Reduce Caries Treatment Expenditures in US Children? Journal of Public Health Dentistry, under 2nd review.
Serban, N., Bush, C., Tomar, S. (Submitted August 2018) Medicaid Capacity for Pediatric Dental Care. Journal of the American Dental Association, under 1st review.
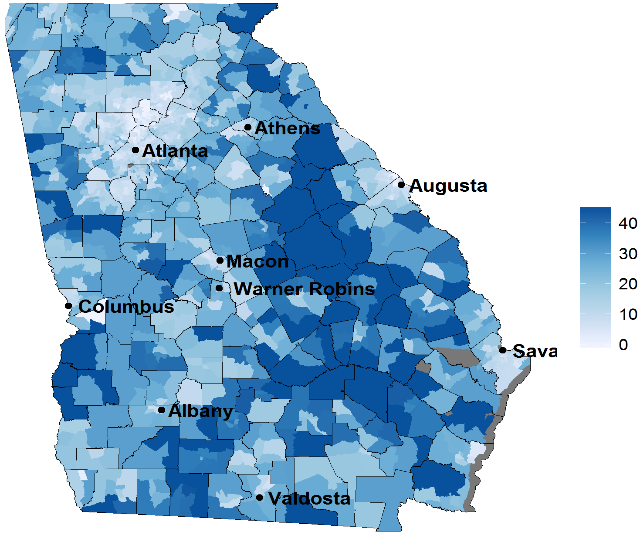
Cao, S., Gentili, M., Griffin, P., Griffin, S., Serban, N. (2017). Disparities in Access to Preventive Dental Care between Publicly and Privately Insured Children in Georgia. Preventive Disease Control, 14:170176.
Cao, S., Gentili, M., Griffin, P., Griffin, S., Harati, P., Johnson, B., Serban, N., Tomar, S. (2017) Estimating demand for and supply of pediatric preventive dental care for children and identifying dental care shortage areas, Georgia, Public Health Reports, 132(3) 343-349.
Johnson, B., Serban, N., Griffin, P., Tomar, S. (2017) The Cost-Effectiveness of Three Interventions for Providing Preventive Services to Low-Income Children, Community Dentistry and Oral Epidemiology, 45(6), 522-528.
Cao, S., Gentili, M., Griffin, P., Griffin, S., Harati, P., Johnson, B., Serban, N., Tomar, S. (2017) "Estimating demand for and supply of pediatric preventive dental care for children and identifying dental care shortage areas, Georgia", Public Health Reports, 132(3) 343-349.
Griffin, S.O., Bailey, W., Brunson, D., Griffin, P.M., Jones, J. (2012). “Burden of Oral Disease among Older Adults and Implications for Public Health Priorities”, American Journal of Public Health, Vol. 102, pp. 411-418.
Griffin, S.O., P.M. Griffin, J. Swann and N. Zlobin (2004). “Estimating Rates of New Root Caries in Older Adults.” Journal of Dental Research, 83(8): 634-638.
Griffin, S.O., Griffin, P.M., Beltran-Aguilar, E.B., Malvitz, D.M., and Heiden, K.D. (2004), “Estimating Prevalence and Severity of Caries in the Mixed Dentition: A Comparison of Two Screening Protocols,” Journal of Public Health Dentistry, Vol. 64, 14-19
Griffin, S.O., Griffin, P.M., Gooch, B.F., and Barker, L.K. (2002), “Comparing the Costs of Three Sealant Delivery Strategies,” Journal of Dental Research, Vol. 81, 641-645
Related Publications
Journals
Nasseh, K. and M. Vujicic (2015). "The Impact of Medicaid Reform on Children's Dental Care Utilization in Connecticut, Maryland, and Texas." Health Services Research 50(4): 1236-1249.
Griffin, S. O., L. K. Barker, L. Wei, C. H. Li, M. S. Albuquerque, B. F. Gooch, C. Centers for Disease and Prevention (2014). "Use of dental care and effective preventive services in preventing tooth decay among U.S. Children and adolescents--Medical Expenditure Panel Survey, United States, 2003-2009 and National Health and Nutrition Examination Survey, United States, 2005-2010." MMWR Suppl 63(2): 54-60.
Ahovuo-Saloranta, A., H. Forss, T. Walsh, A. Hiiri, A. Nordblad, M. Makela and H. V. Worthington (2013). "Sealants for preventing dental decay in the permanent teeth." Cochrane Database of Systematic Reviews.
Hendrix, K. S., S. M. Downs, G. Brophy, C. Carney Doebbeling and N. L. Swigonski (2013). "Threshold analysis of reimbursing physicians for the application of fluoride varnish in young children." Journal of Public Health Dentistry 73(4): 297-303.
Bertrand, E., M. Mallis, N. M. Bui and D. Reinharz (2011). "Cost-effectiveness simulation of a universal publicly funded sealants application program." Journal of Public Health Dentistry 71(1): 38-45.
Sampson, C. (2010). "Is routine dental prophylaxis effective?" Evidence-based dentistry 11(1): 16-17.